Precision Surgery Technologies: How Advanced Tools Transform Modern Medicine
Precision surgery technologies: transform modern medicine
Surgical procedures have evolved dramatically since the days of crude instruments and minimal anesthesia. Today’s operate rooms feature sophisticated technologies that enhance precision, reduce invasiveness, and improve patient outcomes. Among the virtually revolutionary advancements are lasers, robotics, MRI scan capabilities, and genetic research applications — each play a unique role in modern surgical innovation.
Laser technology in modern surgery
Laser technology has essentially transform surgical precision across multiple specialties. Unlike traditional scalpels, lasers offer surgeons the ability to make implausibly precise incisions with minimal damage to surround tissues.
How lasers enhance surgical precision
Lasers work by deliver concentrated light energy to specific tissue areas. This energy can cut, coagulate, or vaporize tissue with remarkable accuracy. The precision come from several key advantages:
- Beam focus angstrom small as 0.1mm — far more precise than conventional cutting tools
- Simultaneous cutting and cauterization, reduce bleeding
- Reduced tissue trauma and inflammation
- Ability to target specific tissue types while preserve others
Applications across surgical specialties
Laser technology has found applications in numerous surgical fields:
Ophthalmology:
Peradventure the virtually substantially know application is last eye surgery, where eexciterlasers reshape the cornea with micrometer precision. Femtosecond lasers have rrevolutionizedcataract surgery by create utterly sized and center capsulotomies.
Dermatology:
Lasers target specific skin conditions with minimal scarring, treat everything from port wine stains to complex skin cancers.
Neurosurgery:
Co2 lasers allow for the precise removal of brain tumors with minimal damage to surround neural tissue.
Gynecology:
Endometriosis and fibroid treatments benefit from the precision of laser techniques that preserve fertility.
The non-contact nature of laser surgery much result in less pain, faster healing, and reduce infection risk compare to conventional methods.
Robotic surgical systems: the pinnacle of precision
Robotic surgery represent one of the virtually significant leaps advancing in surgical precision. These systems translate a surgeon’s hand movements into smaller, more precise actions perform by miniaturize surgical instruments inside the patient’s body.
Components of robotic surgical systems
Modern robotic systems typically consist of three primary components:
-
Surgeon console:
Where the surgeon sit and control the robot use hand and foot controls -
Patient side cart:
The robotic arms that hold instruments and perform the actual surgery -
Vision system:
High definition 3d cameras provide magnify views of the surgical site
Advantages over traditional surgery
Robotic surgery offer several distinct advantages that enhance precision:
-
Tremor filtration:
The system eliminate natural hand tremors, allow for steadier movements -
Motion scale:
Surgeons can adjust the robot to translate large hand movements into microscopic instrument movements -
Enhanced dexterity:
Robotic wrists can rotate 540 degrees, far beyond human capability -
Improved visualization:
10 15x magnification with 3d depth perception -
Ergonomic positioning:
Reduce surgeon fatigue during long procedures
Current applications and limitations
Robotic systems have proved specially valuable in:
Urologic surgery:
Peculiarly prostatectomies, where to enhance precision help preserve nerve function and continence
Gynecologic procedures:
Include hysterectomies and mastectomies, allow for complex dissection in confine spaces
Cardiothoracic surgery:
Enable minimally invasive approaches to antecedently open chest procedures
Colorectal surgery:
Facilitate precise dissection in the narrow confines of the pelvis
Despite these advantages, robotic surgery face limitations include high costs, longsighted setup times, and the need for specialized training. The technology continue to evolve, with newer systems incorporate haptic feedback and autonomous features.
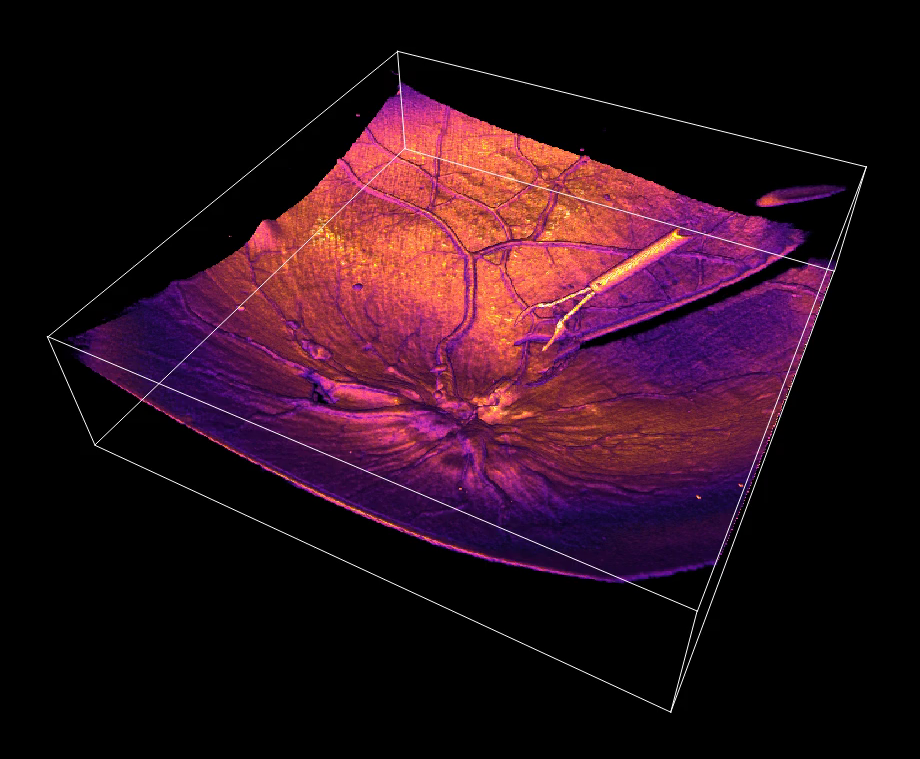
MRI guided interventions: see inside the body
Magnetic resonance imaging (mMRI)has rerevolutionizedurgical precision by allow surgeons to visualize internal structures in unprecedented detail, both before and during procedures.
Pre-surgical planning with mrMRI
High resolution MRI scans provide detailed anatomical information that enable surgeons to:
- Create precise 3d models of patient anatomy
- Identify optimal surgical approaches
- Simulate procedures before enter the operating room
- Reduce unexpected findings during surgery
This planning capability is specially valuable in neurosurgery, where millimeter precision can mean the difference between success and catastrophic outcomes.
Intraoperative MRI
The integration of MRI technology into operating suites has transformed certain surgical procedures:
-
Real time feedback:
Surgeons can obtain update images during procedures -
Confirmation of complete resection:
Specially valuable in tumor removal -
Compensation for brain shift:
Update navigation systems as tissues move during surgery -
Reduced need for secondary procedures:
Confirm successful treatment before close
MRI compatible surgical tools
The development of MRI compatible instruments has enabled interventions within theMRIi environment:
- Non-ferromagnetic materials that won’t be will affect by the magnetic field
- Special surgical navigation tools that function in high field environments
- Robotic systems design specifically for MRI guide procedures
MRI guidance has proved specially valuable in procedures target the brain, breast, prostate, and liver, where soft tissue visualization is critical for precision.
Genetic research: personalize surgical approaches
While peradventure less visible in the operating room itself, genetic research has begun to transform surgical precision through personalize approaches base on individual genetic profiles.

Source: dreamstime.com
Pharmacogenomics in surgical care
Genetic testing straightaway informs medication choices throughout the surgical journey:
- Predict individual responses to anesthesia
- Optimize pain management protocols
- Identify patients at risk for adverse drug reactions
- Tailor anticoagulation therapy
These personalize approaches reduce complications and improve outcomes by account for genetic variability.
Tumor genomics and precision oncologic surgery
Cancer surgery has been revolutionized by genetic insights:
-
Targeted resections:
Genetic profiling help determine optimal surgical margins -
Intraoperative molecular testing:
Rapid genetic analysis during surgery guides decision make -
Fluorescence guide surgery:
Genetic markers help visualize tumor boundaries -
Neoadjuvant therapy selection:
Genetic profiles inform pre-surgical treatments
These approaches ensure that surgery is just tailored to the individual tumor’s biology preferably than follow one size fit all protocols.
Future directions in genetic surgical applications
Emerge technologies promise eventide greater precision:
- CRISPR base surgical adjuncts to modify tissues during procedures
- Genetically target drug delivery systems activate during surgery
- Personalized tissue engineering base on genetic profiles
- Predictive models for surgical outcomes base on genetic factors
Integration of multiple technologies
The virtually significant advances in surgical precision oftentimes come from combine these technologies into integrated systems.
Hybrid operate rooms
Modern hybrid ORS integrate multiple imaging and intervention technologies:
- MRI or ct scanners with robotic surgical systems
- Fluoroscopy with laser ablation capabilities
- Ultrasound guidance with robotic assistance
- Augmented reality overlay with genetic information
These integrate environments allow seamless transitions between imaging, planning, and intervention.

Source: medical.robotics.umich.edu
Artificial intelligence and machine learning
Ai systems are enhanced precision across surgical technologies:
- Analyze MRI data to identify structures invisible to the human eye
- Provide decision support during robotic procedures
- Correlate genetic information with optimal surgical approaches
- Predict complications before they occur
These systems act as an additional layer of precision, augment human capabilities instead than replace them.
Patient benefits of precision surgery
The ultimate measure of surgical precision is patient outcomes, which have improved dramatically:
Reduced complications
- Lower infection rates due to smaller incisions
- Reduced blood loss from precise vessel management
- Fewer unintended injuries to adjacent structures
- Decrease anesthesia relate complications from shorter procedures
Improved functional outcomes
- Better preservation of normal tissue function
- Reduced scarring and adhesions
- Faster return to normal activities
- Improved cosmetic results
Access to antecedently impossible procedures
- Surgery on antecedently inoperable deep brain tumors
- Precision repairs of microscopic structures
- Minimally invasive approaches to complex anatomical regions
- Interventions tailor to rare genetic conditions
The future of precision surgery
Look leading, several emerge technologies promise to far enhance surgical precision:
Autonomous surgical systems
While full autonomy remain distant, semi autonomous systems are emerged that can perform specific surgical tasks with superhuman precision, such as suture blood vessels or remove incisively define tissue volumes.
Nanotechnology
Microscopic surgical tools deliver through the bloodstream may finally allow for cellular level precision, target individual diseased cells while leave healthy tissue untouched.
Telerobotic surgery
Remote surgical capabilities are expanded, potentially allow specialists to provide precision surgical care irrespective of geographic limitations.
Conclusion
The evolution of surgical precision through lasers, robotics, MRI guidance, and genetic research has transformed modern medicine. These technologies, peculiarly wheintegratedte, allow surgeons to perform procedures with accuracy that would haseeneem impossible precisely decadaloneone.
As these technologies will continue to will advance and become more accessible, patients worldwide will benefit from reduced complications, improved outcomes, and access to life will change procedures. The future of precision surgery promise tied greater capabilities, with emerge technologies potentially revolutionize our approach to surgical intervention at the cellular and molecular levels.
For patients and healthcare providers likewise, understand these precision technologies help inform decisions about surgical options and highlights the importance of seek centers with access to these advanced capabilities when complex procedures are need.