Health Education: Complete Guide to Promoting Wellness Through Knowledge
What’s health education?
Health education is the systematic process of teach individuals and communities about health relate topics to improve knowledge and develop life skills that support personal and community health. It encompasses plan learning experiences design to help people make informed decisions about their wellbeing.
Unlike simple health information sharing, comprehensive health education empower people to translate knowledge into positive health behaviors. It addresses physical, mental, emotional, and social dimensions of health while consider factors like environment, culture, and socioeconomic status.
Core principles of health education
Effective health education stand on several fundamental principles:
Evidence base approach
Health education rely on scientific research and prove methodologies. Programs incorporate current medical knowledge and behavioral science to ensure information accuracy and effectiveness. This evidence base foundation distinguishes quality health education from potentially harmful misinformation.
Empowerment and autonomy
Preferably than dictate behaviors, quality health education equip individuals with knowledge and skills to make their own informed choices. This autonomy center approach recognize that sustainable health behaviors emerge when people understand their options and feel confident in their decision make abilities.
Cultural relevance
Effective health education respects and incorporate cultural perspectives, beliefs, and practices. Programs must adapt to diverse populations, consider language, values, and cultural context to ensure messages resonate with intended audiences.
Holistic perspective
Health education acknowledge the interconnectedness of physical, mental, emotional, and social wellbeing. Programs address this full spectrum instead than focus exclusively on disease prevention or physical health.
Key settings for health education
Health education occur across various environments, each offer unique opportunities to reach different populations:
Schools and academic institutions
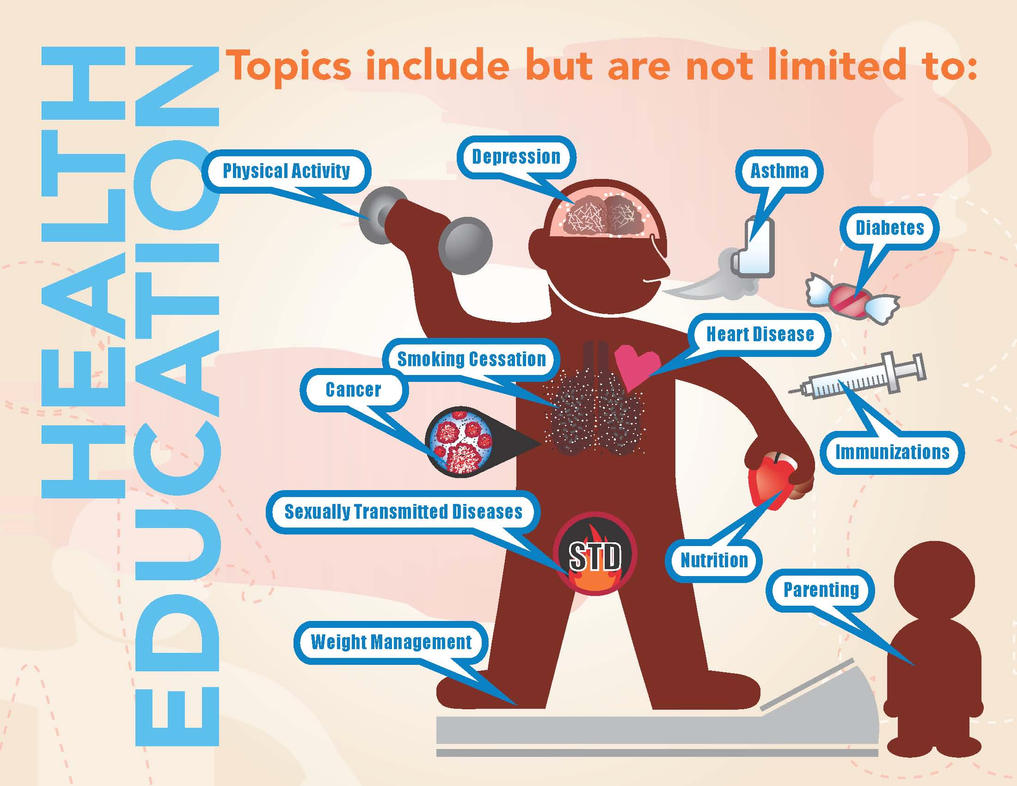
School base health education provide a foundation for lifelong health literacy. Comprehensive programs cover topics like nutrition, physical activity, mental health, substance abuse prevention, and sexual health. The structured environment allows for sequential learning that build knowledge and skills increasingly.
Effective school health education extend beyond traditional classrooms to include cafeterias, playgrounds, and after school programs, create a health promote environment throughout the educational experience.

Source: slideserve.com
Healthcare settings
Hospitals, clinics, and medical offices serve as critical venues for health education. Healthcare providers deliver personalized education during appointments, while specialized health educators may conduct group sessions on chronic disease management, preventive care, or specific health conditions.
Patient education materials, from brochures to digital resources, complement in person education. The healthcare set allow for tailored information delivery at teachable moments when patients are about receptive to health guidance.
Community organizations
Community centers, religious institutions, and non-profit organizations reach populations that may have limit access to other health education sources. These settings frequently address specific community health concerns through workshops, support groups, and outreach programs.
The effectiveness of community base health education stem from trust relationships and cultural alignment with local populations. Programs can address social determinants of health alongside traditional health topics.
Workplace programs
Workplace health education reach adults where they spend significant time. Programs may include wellness workshops, health screenings, ergonomic training, and stress management resources. The workplace set allow for ongoing reinforcement of health messages and creation of supportive environments for behavior change.
Digital platforms
Online resources, mobile applications, and social media have transform health education accessibility. These platforms offer on demand information, interactive learning experiences, and virtual support communities. Digital health education reach populations disregarding of geographic location and provide anonymity for sensitive topics.
Essential components of health education programs
Comprehensive health education programs incorporate several key elements:
Health literacy development
Health literacy encompass the ability to obtain, process, and understand basic health information need to make appropriate health decisions. Education programs build these skills through clear communication, interactive learning, and practical application of health concepts.
Strategies include teach people how to evaluate health information sources, understand medical terminology, navigate healthcare systems, and communicate efficaciously with healthcare providers.
Behavior change techniques
Knowledge solely seldom change behavior. Effective health education incorporate evidence base behavior change techniques like goal setting, self monitoring, skill building, and reinforcement strategies. Programs help participants identify barriers to healthy behaviors and develop practical solutions.
Skill development
Beyond information delivery, health education build practical skills through demonstration, practice, and feedback. These may include:
- Decision-making and problem solve skills
- Communication and refusal skills for peer pressure situations
- Stress management techniques
- Self-care practices for chronic condition management
- Food preparation and physical activity skill
Advocacy training
Many programs teach participants to advocate for health supportive environments and policies. This might include community organizing skills, understand policy processes, or communication strategies for health advocacy.
Health education approaches and methodologies
Several theoretical frameworks guide health education practice:
Social cognitive theory
This approach emphasize the interaction between personal factors, environmental influences, and behavior. Programs base on social cognitive theory focus on build self-efficacy (confidence in one’s ability to perform behaviors ) provide opportunities for observational learning, and create supportive environments.
Health belief model
This model suggest that health behaviors depend on perceive susceptibility to health problems, perceive severity of consequences, perceive benefits of action, perceive barriers, and cues to action. Education programs address these perceptions to motivate behavior change.
Transtheoretical model
To know as the stages of change model, this approach rrecognizesthat behavior change occur through a series of stages: precontemplation, contemplation, preparation, action, and maintenance. Effective programs tailor strategies to an individual’s current stage.
Ecological models
These frameworks consider multiple levels of influence on health behaviors, from individual factors to family, community, and policy environments. Programs base on ecological models address multiple levels simultaneously for maximum impact.
Health education specializations
Health education encompass numerous specialized areas:
Nutrition education
This specialization focus on healthy eat patterns, food preparation skills, and understand nutritional information. Programs address topics like portion control, read food labels, meal planning, and cultural food traditions.
Sexual health education
Comprehensive sexual health education cover reproductive health, healthy relationships, consent, contraception, and disease prevention. Evidence base programs provide medically accurate information appropriate to developmental stages.
Substance abuse prevention
These programs address alcohol, tobacco, and other drug use through risk awareness, refusal skills, and healthy cope alternatives. Effective approaches consider social influences and environmental factors contribute to substance use.
Mental health education
This grows area focus on emotional wellbeing, stress management, recognize mental health conditions, and reduce stigma. Programs build resilience skills and increase awareness of mental health resources.
Chronic disease management
Education for conditions like diabetes, heart disease, or asthma help patients understand their condition, manage symptoms, follow treatment plans, and prevent complications. Self-management education empower patients to take active roles in their care.
The role of health educators
Professional health educators serve as specialists in promote health through educational strategies. Their responsibilities typically include:
Need assessment
Health educators analyze community or population health need through data collection, surveys, interviews, and demographic analysis. This assessment inform program development and resource allocation.
Program planning and implementation
Base on identify needs, health educators design, coordinate, and deliver educational programs. They select appropriate teaching methods, develop materials, and create evaluation plans.
Evaluation and research
Measure program effectiveness through both process and outcome evaluation help refine approaches and demonstrate impact. Health educators may conduct research to advance the field’s evidence base.
Resource development
Create accessible, accurate educational materials require translate complex health information into understandable formats. Health educators develop print materials, digital resources, presentations, and interactive tools.
Advocacy and policy development
Many health educators work to create supportive environments through policy initiatives, community organizing, and institutional change efforts.
Impact and outcomes of health education
Effective health education generate measurable benefits at individual and community levels:
Individual health outcomes
Research demonstrate that quality health education contribute to:

Source: slideserve.com
- Improved health knowledge and literacy
- Adoption of preventive health behaviors
- Better management of chronic conditions
- Increase utilization of appropriate healthcare services
- Enhanced quality of life and well bee
Community and public health impact
At broader levels, health education contribute to:
- Reduced healthcare costs through prevention
- Decrease health disparities when programs reach underserved populations
- Increase community capacity to address health challenges
- Development of health supportive environments and policies
- Improved population health indicators
Challenges in health education
Despite its importance, health education face several challenges:
Misinformation and competing messages
The proliferation of health misinformation, peculiarly online, create confusion and undermines evidence base education. Health educators must help people develop critical evaluation skills for health information sources.
Access and equity issues
Health education resources oftentimes fail to reach those with greatest need due to geographic, economic, linguistic, or cultural barriers. Address these disparities require innovative delivery methods and culturally tailor approaches.
Measure long term impact
Health behavior change occur gradually, make it challenge to measure program effectiveness. Develop meaningful evaluation strategies that capture both immediate and long term outcomes remain difficult.
Resource limitations
Many health education programs operate with insufficient funding, staffing, and materials. Demonstrate return on investment help secure necessary resources for sustainability.
Future directions in health education
The field continue to evolve in response to change health needs and technological advances:
Digital and mobile health education
Technology enable personalize, accessible health education through smartphones, wearable devices, and interactive platforms. Virtual reality, gamification, and artificial intelligence offer promise approaches for engagement and behavior change.
Integration with healthcare delivery
Health education progressively integrates with clinical care through patient portals, telehealth, and team base approaches. This integrationcreatese opportunities for reinforce learning and coordinated support.
Focus on social determinants
Recognition that health outcomes depend mostly on social, economic, and environmental factors has expanded health education to address these determinants alongside individual behaviors.
Personalized approaches
Tailor education to individual needs, preferences, learn styles, and readiness for change improve effectiveness. Advances in data analytics support progressively personalize educational experiences.
Conclusion
Health education serve as a cornerstone of public health and healthcare delivery, empower individuals and communities with knowledge and skills for well bee. Beyond simple information transfer, effective health education build capacity for informeddecision-makingg and sustainable behavior change.
As health challenges evolve, hence also must health education approaches. Will embrace technological innovations, will address social determinants, and will ensure equitable access will strengthen health education’s impact. By foster health literacy and self-efficacy, health education contribute to the broader goals of disease prevention, health promotion, and healthcare quality improvement.
Whether deliver in schools, healthcare settings, workplaces, or digital environments, quality health education represent an essential investment in human potential and population health. Its continued development and implementation remain vital to address current and emerge health challenges.